Thomas E. Levy, MD, JD, is a board-certified cardiologist and attorney. He was inducted into the Orthomolecular Medicine Hall of Fame in 2016. According to Dr. Levy, all root canal-treated teeth are infected and toxic. In this article published in JOM ion November 1, 2016, Oral Pathogens: A Common Cause of Chronic Disease, he wrote:
And while no part of the body can completely avoid the regular delivery of these toxic pay-loads, they are especially prone to go via the lymphatics into the chest, neck and head. The venous drainage ends up impacting especially severely the coronary and carotid arteries.
And I stopped.
Hidden Symptoms of Tooth Infection
And I thought about my history of mysterious health complaints and chronic diseases ever since a root canal was performed on my lower left molar over 20 years ago when I was in my 20s.
- Hair loss that regularly clogged the shower drain
- Irritability
- Regular sinus infections
- Constant red, runny nose
- Frequent sore throats with fever
- Painful neck and shoulders
- Hypothyroidism diagnosis in 2006
- Heart palpitations
- Unusually dense breasts detected at my first mammogram age 40
- A full-body thermography showed my entire head, neck, and chest lit up like a Christmas tree from inflammation
But let’s think for a minute about all the possible health complaints that could develop if those pathogens traveled to the head, neck, and chest regions.
Head Symptoms: Damaged, frizzy, flakey, itchy, thinning hair, mental health conditions, irritability, mood swings, brain fog, attention deficit disorder, ADHD, learning disabilities, dementia, sinusitis, running nose, problems with the eyes and ears, coating on tongue, bad breath, mouth sores, gingivitis, tooth decay, gum disease, loose teeth, facial pain, tooth pain, headaches, migraines, fever
Neck Symptoms: Thyroid disease, throat infections, tonsillitis, difficulty swallowing or taking a deep breath, thyroid cancer (and all forms of cancers of the the head, neck, and chest), neck or shoulder pain
Chest Symptoms: Dense breasts, breast cysts, heart disease, lung disease, chronic bronchitis, pneumonia, emphysema
I visited a biological dentist in New York City 5 to 10 years ago. He said, “Your dental x-rays look fine but I have a hunch that you have an infection at your root canal site. You should have your tooth extracted.”
Now that sounded so extreme, and so out of the blue, especially given my x-rays never showed a problem. I had no pain of any kind and no visible problems with that tooth. It looked perfectly normal. Plus I had read all about the hot bed of debate among the dental community on unnecessary extraction of root canal teeth. On top of it all, I didn’t want to walk around with a missing tooth and then worry what to do to safely replace it.
To extract a perfectly normal tooth with no evidence but a person’s hunch just seemed like too much. Besides, the official position of the American Association of Endodontists is that root canals are safe, after all.
I decided to keep my tooth.
If I was going to ever extract that tooth, I wanted proof, hard proof. Period.
My “Asymptomatic” Tooth
The more and more I read about the topic over the years, the more and more my gut instinct started whispering and then shouting that something was wrong with my tooth.
I went to one dentist after another that told me my tooth looked fine on standard dental x-rays and I was not symptomatic for dental infection.
I had read about panorama x-rays. It is a 2-dimensional dental x-ray that takes a wide view of the teeth, jaws and surrounding structures. You see standard dental x-rays don’t capture what’s outside the capabilities of the imaging equipment, and that includes below the roots of the tooth deep in the jaw bones.
You see a healthy oral cavity is colonized by diverse “good” microorganisms and the oral microbiome is considered the second most complex microbiome in the human body, following that of the colon. Serious problems develop when the normal oral microbiota gives rise to opportunistic pathogens, including bacteria, viruses, and fungi. These opportunistic pathogens can get access to the dental pulp tissue within teeth through openings in the hard enamel whose role is to prevent entry to the interior of the teeth. Oral pathogens can pass the enamel through cavities, cracks, or traumatic injuries to the teeth. In my case, I fractured that tooth when I was a little girl from grinding my teeth and then that tooth by my 20s got infected and was given a root canal.
In an ideal world, every root canal procedure would reach and eradicate all the pathogens within the tooth. I assumed this to be the case, but the more I dug into this topic the more I understood. Even when done perfectly by an expert dentist there is always the possibility that the root canal treatment fails to get all of the pathogenic microorganisms present. There are many possible hiding places for microorganisms in those roots, accessory canals, and complex dentin tubules. Plus some microorganisms have developed resistance to antimicrobial treatment and can survive the sterilization procedures performed in a standard root canal. This study here showed that even when all the pathogens are removed during a root canal procedure, the endoctoxins that they release may still be present. And here’s another point. There is always the possibility that a completely sterilized root canal tooth can get re-infected.
In a study published in May 2019, researchers identified the microbiota associated with endodontic (root canal) failure as well as the reasons why these microorganisms are capable of surviving disinfection measures. They wrote:
These microorganisms have in common the following proprieties, which make them able to escape the disinfection measures: the ability to form a biofilm, to locate in areas unreachable to root canal instrumentation techniques, synergism, the ability to express survival genes and activate alternative metabolic pathways.
Enterococcus faecalis is one of the most commonly identified microoganism associated with endodontic failure, although there are many different bacteria, fungus, viruses, and even parasites that can breed in our root canal teeth. E. faecalis is a Gram-positive facultative anaerobe that naturally inhabits healthy human GI tracts but it can develop into an opportunistic pathogen in root-canal teeth. It is also a common pathogen in hospital-acquired infections. It can cause enocarditis and sepsis, urinary tract infections (remember my history of UTIs!), and meningitis.. E. faecalis is multi-drug resistant to many different antibioitics which makes it difficult to treat and it is not a far leap to guess that it may also be resistant to the standard root canal disinfectant materials.
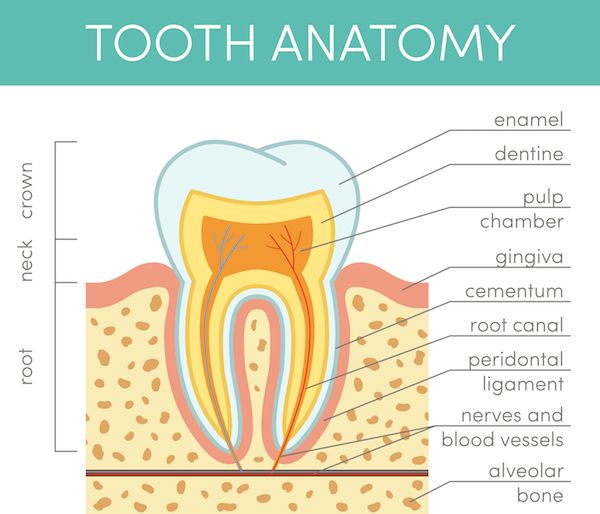
During the root canal procedure, the tooth is cut off from the blood and lymph supply thereby cutting off the paths to bring immune cells into the tooth and to carry waste out. Neither the body’s immune system nor antibiotics can reach within this root canal tooth and those little bugs within it go on their merry way breeding like rabbits with nothing in their way. Imagine that infected root canal like a water tap stuck “on” with pathogens flowing out of it every every second of every day for years, and even decades for some people, making their way around the body. The reality is that a root canal tooth is a “dead” tooth and I’m not sure how having a dead thing in your body can be such a good idea.
Oral Pathogens & My Thyroid
Yes the immune system can fight the pathogens once they have migrated outside the root canal space where they can be reached by antibodies traveling through the blood stream but just imagine how a constant flood of “foreign” invaders would over time weaken the immune system and even set the stage for autoimmune disease like Hashimoto’s thyroiditis and Grave’s disease. Think of the root canal tooth as an ant hill and “the ants go marching two by two, hurrah, hurrah”. It sounds so cute in a children’s song but not so cute when bad bugs are marching out of my tooth towards organs more than likely, I have a hunch, to the weakest links in my body. The immune system can only handle this non-stop onslaught for so long before it breaks down. It’s just a matter of time.
A 2018 Yale University study discovered that bacteria in the small intestines can travel to other organs and trigger an autoimmune response. This concept that pathogens can travel around the body is what got my wheels turning to write this article.
I had my root canal for over 20 years so just imagine the number of years that those bad bugs were growing and replicating in my darn tooth and then traveling to my nearby head, neck (yup I’m sure my thyroid was a target) and chest regions, not to mention to other body parts, in my case to my bladder (oh the terrible recurring UTIs began at about that same time), by taking a ride through our blood stream and lymphatic system. The immune system is designed to protect the body from danger, but sometimes that survival mechanism can go astray. Imagine, for example, the bad bugs from your root canal reach your thyroid gland. Your immune system has tagged that bug as an invader that it needs to destroy and, while it tries to eradicate the bug, it can also mistakenly destroy portions of the thyroid gland (an innocent bystander) where the bug is hiding.
It is really a vicious cycle. And then comes the question, “Which came first, the chicken or the egg?” One of the classic signs of hypothyroidism is chronically low body temperature. That low body temperature makes the chronically ill hypothyroid person’s body a haven for bugs. This explains too how vulnerability to infections in all different body parts – sinuses, ears, eyes, throat, lungs, intestines, vagina, bladder, feet, and teeth – goes hand in hand with low thyroid.
There is no blame here. I know how serious this topic is for everyone. We make the best decision we can at the time with what we know. My hope is that this article gives you new information to help you make the best decisions for your own teeth.
Dental Pathogens Tricky to Detect
The decision to extract my tooth was one that took years for me to decide and a decision that I did not take lightly.
I also limit my exposure to radiation whenever possible including dental x-rays and that meant making a decision about the panoramic x-ray as well. The less unnecessary exposure the better, right. I weighed the pros and the cons and after all that I knew about the topic, I felt it was the right decision to make in my case.
It is important to add here the importance of thyroid safety when it comes to taking dental x-rays. Be sure that a thyroid collar (also known as a thyroid shield) is used during dental x-rays. Your dental office may have led aprons with built-in thyroid collars or as a separate collar to add to it. In 2012, the American Thyroid Association released a policy statement about minimizing risks to the thyroid gland association with radiation exposure from diagnostic medical and dental radiography.
Radiation exposure to the thyroid among both children and adults is currently the strongest known risk factor for thyroid cancer.
Thyroid-protective collars should be used for all dental x-rays when they do not interfere with the examination.
The American Thyroid Association also published a study in 2017 titled Childhood radiation and thyroid cancer. The authors found that thyroid cancer was more common in individuals who had a history of radiation exposure to the head and neck areas as children.
I searched my area online for dentists that offer the panormic x-ray. Not all dental offices carry this technology.
My dentist pointed at the panoramic x-ray results and there below the root tips of my root canal tooth was a major, visibly huge even to my untrained eyes, infection that descended down my jaw bone. The infection was missed for years of going from dentist to dentist taking one standard dental x-ray after another and every dentist reporting that my tooth was perfectly fine. He put up my recent standard dental x-ray to compare it to the panoramic and everything made sense.
The standard x-ray only showed a view just below the root tips of my teeth but this infection was just below that and spread out in a large formation in my jaw and that was the reason it was never detected, until now.
Those little monster bugs had eaten their way through the bone under that tooth and were on their way to the adjacent bone. I might have started losing teeth from all of this if I hadn’t discovered the stealth infection with this panoramic x-ray.
By the way, root canal teeth are not the only source of dental pathogens that are important to consider here.
Other Sources of Dental Pathogens
Dental implants.
More than 5 million dental implants placed each year in the United States. Researchers have uncovered the significance of microbial biofilms associated with all types of implanted medical devices including tooth implants. Microbes gather in formation into what is termed “bioofilms” as a means of survival. Imagine the little bugs all gathering into a ball, for a moment, the body’s immune system forms antibodies to attack foreign particles including bad bugs but the bugs buried deep within the ball evade attack from the immune system and even antibiotics can’t reach them inside the ball. Here’s the scary thing. Implanted medical devices including not just dental implants but also catheters, artifiical valves, joint replacements, cardiac pacemakers, and stents provide an ideal environment for colonization. Even the dental plaque that we get cleaned off the surfaces of our teeth during routine dental visits are biofilms. Those bugs are seriously smart. They know how to survive and outwit us.
It goes without saying that everyone should regularly brush, floss, and get dental cleanings. I’ve added a tongue scraper to my daily routine to remove the tongue coating that can develop from buildup of microorganisms and can contribute to bad breath. I also use a waterpik with salt added to the water or just rinse your mouth with salt water. I mix salt and baking soda with a touch of water to make a paste and apply it to my gums with a toothbrush for a minute before rinsing off. I don’t use baking soda regularly because of the abrasiveness of it but from time to time. Remember that pathogens can move from your mouth to your toothbrush and vice versa. If you’ve been using the same toothbrush for 5 years, throw it out and buy a new one. Make a routine of buying new toothbrushes for yourself and your family members, including children, every so often. In between, keep your tooth brush clean. Don’t place it on the dirty bathroom counter or bristles down in a dirty toothbrush holder. Regularly clean your toothbrush too. I put my toothbrush bristles down in a clean glass and cover the tip with bristles with salt and leave it for an hour.
You can also try the ancient Ayurvedic practice of “oil-pulling”. I use dentist Dr. Carey O’Rielly’s tip of adding 2-3 drops of oil of oregano in 1 tablespoon of cold pressed organic olive oil and swish it around my mouth for a few minutes and spit it out. The idea is that it pulls out the toxins including the pathogens so you don’t want to swallow this. Dr. O’Rielly has a holistic dental practice in Encinitas, California. In this video, he explains how salt kills the bacteria in your mouth.
Killing Bacteria Naturally with Salt
To complicate things further when it comes to medical devices is the fact that many of us are sensitive to one or more types of metals and plastics used in those medical devices. Titanium dental implants are the most common type yet titanium allergy is a real concern. Titanium contains traces of nickel and nickel allergies are pervasive and can develop at any age. Nickel is used in crowns, bridges, partial dentures, and orthodontic appliances like brackets and retainer wire. Zirconia implants are an alternative. They are advertised as metal-free, chemically unreactive ceramic. Although truth be told, we can be sensitive to all types of materials, metal or ceramic or any other material. There are dental material compatibility tests, like the Clifford Materials Reactivity Testing and MELISA Test, available to test a broad range of dental materials to determine which materials are biocompatible with the patient’s unique biochemistry.
Orthodontics.
Did you get sick during or soon after you had braces? I was startled to read these words from researchers in a 2014 study:
Improved preventive measures and antimicrobial materials are urgently required to prevent biofilm-related complications of orthodontic treatment from overshadowing its functional and estehtic advantages. High treatment demand and occurence of biofilm-related complications requiring professional care make orthodontic treatment a potential public health threat.
Periodontal disease.
One plausible cause of gum disease, also known as periodontal disease, is colonization of microbes in the mouth, including the dental plaque biofilms on tooth surfaces. The body’s immune system goes into a hyper-response to attack the microbes that are tagged as “foreign” resulting in chronic inflammation of the gums and even eventual gum recession and loosening of teeth. It is important to note that we all have symbiotic microbes (good bugs) as part of the normal flora in our mouth. Actually we have microorganisms all over the outside and inside of our bodies and some provide benefits including some oral bacteria that can protect us from tooth erosion. Not all bugs are bad, all the time. You just have to look at the long list of newly identified pathogens associated with periodontitis to know that there are definitely bad oral bugs too, all kinds of them.
Dentures.
Researchers estimate that 20% of the UK population wear some form of denture prosthesis and half of these individual develop denture stomatitis. Candida albicans (an insidious yeast) is the primary cause due its biofilm-forming ability. In this study, different types of popular denture cleaners were tested. Antimicrobial denture cleaners do not fully eradicate C albicans. In another study, the importance of daily removal of the denture biofilm including both mechanical cleaning in conjunction with immersion in denture cleansers is advised. “Complete denture biofilm is defined as a dense layer of complex microbial communities embedded in a polymeric matrix, and it is known to contain more than 1,011 microorganisms by gram in dry weight.” With what I wrote above about the power of salt to kill microorganisms, immerse your dentures in warm salt water as an added cleaning step or add salt to the denture cleaner directly.
Extraction of My Root Canal Tooth
My extraction was done with a biological dentist. I did an online search for “holistic dentist” and “biological dentist” in my area and surrounding areas. I called each office, one by one. I went in as an informed patient and I hope the same for you should you find yourself in a similar situation.
Here are 2 important questions that I asked:
1. Will the extraction include removal of the periodontal ligament?
The periodontal ligament is a group of specialized connective tissue that connects each tooth with the walls of the tooth socket and anchors it to the jaw. Given the ease with which pathogens travel in the body, it makes sense that the bugs in an infected root canal tooth would travel to the surrounding areas including the periodontal ligament. Extraction of my tooth would require a knowledgable doctor who would also remove that periodontal ligament and infected bone.
There’s another important reason to extract the periodontal ligament.
Jaw bone cavitations.
Standard tooth extraction, including extraction of wisdom teeth, may omit this important step. According to the Weston A. Price Foundation:
The primary cause of these jawbone cavitations in extraction sites is the failure of the convention dentist or oral surgeon to remove all of the periodontal ligaments when pulling a tooth. Dr. Hal Huggins likens the severity of this dental omission to the failure of removing the placenta (afterbirth) after delivery a baby.
If the periodontal ligament is not removed after the extraction, the surrounding bone does not receive the biological message that the tooth is gone and that new jaw bone growth is needed. That void, that hole, in the jaw bone is called a cavitation. These holes have impaired blood flow so they are filled with dead tissue making it a perfect breeding ground for pathogens and the toxins they secrete and both seep into the body. This impaired blood flow also means that immune cells and antibiotics have a hard time reaching within these holes to eradicate the bugs. Cavitations can cause facial pain but they can also be “asymptomatic” with bizarre, seemingly unrelated symptoms far removed from the original source of infection. Think head, neck, chest, but also the rest of the body.
When researchers explored extraction sites for cavitations, cavitations were found in 75% of all extraction sites in the mouth and in 88% of wisdom tooth extractions specifically.
Dr. Weston A. Price was a renowned dentist in the early 1900s. He began to suspect that root canal teeth were causing chronic diseases in his patients, including one woman who was in a wheelchair due to severe arthritis. The tooth looked “normal” with no evidence of infection on x-rays. He extracted her root canal tooth and implanted it under the skin of a healthy rabbit. Within 48 hours that rabbit was crippled with arthritis. In 10 days, the rabbit died.
2. What is your treatment protocol for the prevention and/or treatment of pathogens that spread from the extraction site?
Reported cases in the scientific literature of dental infection spreading to the brain date back to 1985. In 2013, the Canadian Dental Association published a case report of a 30-year-old man, reportedly in good health before his dentist completed a root canal on his molar. The next day the man called his dentist to complain of facial swelling and pain and was prescribed amoxicillin and moderate strength analgesic. The symptoms increased over 48 hours and he had lost vision in his left eye. He was admitted to the hospital for eye infection and died several hours after admission. And this reminds us all to speak to our dentists always before serious dental work, especially in cases of known infections, about their approach to treating pathogens that may spread through the body.
The American Association of Endodontists recommends antibiotic use in endodontic treatment in special cases including patients at risk of infective endocarditis or prosthetic joint implant infection, as well organ and stem cell transplant patients.
I am generally cautious about antibiotic use because wiping out my beneficial gut bacteria would then also leave me vulnerable to infestation of opportunistic organisms. Keeping a strong gut flora is particularly important should an infection in my tooth travel down to my gut. Every case is different, however, and it is essential to discuss what steps your dentist will take especially what steps they recommend you take should you develop signs of infection post-treatment. There are alternatives to antibiotics and seeking multiple opinions from different dentists including biological dentists can help you make an informed decision. Alternatives to discuss include Leucocyte and Platelet Rich Fibrin (L-PRF), Pure-Platelet-Rich Plasma (P-PRP), ozone water, topical ozone oil, intravenous vitamin C.
Tooth Infection & Hair Loss
Soon after my tooth extraction, I started to notice more energy. And my face, it began to have more color, less pale and sickly, with a healthy glow.
The thyroid hormone medication dosage that was ideal for me the past 6 years was all of a sudden more than my body needed. Hyperthyroid-like symptoms began and my thyroid dosage needed to be reduced. I’m feeling great at this lower dosage.
This past summer I went in for my third full-body thermography (I’ve been getting them done every few years and I tell my thermography story here.) Going over my latest results and comparing them with my past results, one thing jumped out off the pages. The red hot inflammation all over my head (in particular my mouth and sinuses), neck, and chest had dramatically reduced. The technician said, “You had the highest inflammation in the lower left gum line in past results but now there is zero detected. What have you done?” Remember that my root canal was on a lower left molar.
But, there was something else and this blew me away.
One of the most popular articles at Hypothyroid Mom is 10 Things That Stopped My Thyroid Hair Loss. My massive thyroid hair loss dramatically reduced thanks to those 10 things that I wrote about in 2014, but this tooth extraction did something dramatic.
I’ve been counting the number of hairs that fall with every shower every day now for years. I started doing this when the hair started falling out in big mounds and I was seriously worried. According to the American Academy of Dermatology, it is normal to lose 50 to 100 strands of hair per day. So I started counting. I was up to about 300 hairs a day at my worst. And thanks to the 10 things that I listed in my article I was down to about 80-100 strands of hair loss per day. I was ecstatic. My thinning areas were filling in and my hair was looking less like a dry hay stack.
But, I had no idea that it could get even better than that.
Over the last several years I’ve been experimenting with even more hair loss treatments and several that are bizarre, really, not what I expected at all made a big difference. I’ve been counting the hairs that fall out every day when I shower in a way to see if I can quantify what things that I’ve tried are working and what’s not working. Stay tuned because I plan to share my findings over the next few months at Hypothyroid Mom. Thanks to these things my hair loss reduced down to about 60-80 strands of hair loss per day.
This is “normal” daily hair loss according to the American Academy of Dermatologist. And my hair was visibly thicker and more voluminous.
But, I still had no idea that it could get even better than that.
One morning a few weeks after my tooth extraction, I counted my hairs after my shower like I always do.
30.
I thought it must be some mistake. Some hair must have fallen down the drain or on the floor or it was a fluke. It must be.
Day after day for the last 9 months since my extraction, I have been down to 20-50 strands of hair loss per day.
A far cry from the 300 when I feared that I might go bald. Better than the 80-100. And even better than the 60-80.
“Hey Dana, your hair is so shiny.”
“And so healthy.”
“Did you do something different to your hair?”
“No,” I reply. “I got my infected root canal tooth pulled out, finally.”

My GP drew routine lab work. This occurred many years ago. He said that I had a thyroid problem. There was a small lump on (R) side of neck. I have been to an endocrinologist. He did a biopsy that was negative but said that I have Hashimoto’s Disease. I went back several times until he was satisfied that I was on the correct dose of levothyroxine. Had a repeat sonogram and the lump was very much smaller. But…I have had tooth problems my entire life. I am getting ready to have my teeth removed and a mouth full of implants. I need to know if this is safe. I am over 65 years old, have some minor cardiac issues and am scared. My husband recently passed, so my support person is gone. Dana…can you help me? Almost every tooth in my mouth has been root canaled and crowned. They started decaying @ the gum line in the back of the tooth. My husband was ill, so I didn’t notice. They didn’t hurt. I don’t want to make a bad situation worse. I know for sure that a top front tooth is infected presently. I am the only one to care for myself and my dogs. Help!
This is almost spooky! Over the past 3 years I have been having issues with two upper teeth. I was told nothing was wrong over and over. Until, with quick onset, I had horrible pain in my jaw, ear, throat, and then it went down into my chest. Had this not been on my right side I would have suspected I was having a heart attack… it was incredibly scary. I was sent for root canal. All symptoms resolved except my jaw pain. The area was squishy- it had some give, and very painful. I was assured it was all good! (?I knew that pain was not my imagination- I don’t know why I didn’t push the issue?!?) that was a year ago. One month ago I began having the same intense pain from ear to chest. 🌼this time I was sent for panoramic study which clearly showed incredible infection that had indeed eroded my jaw bone!!!!!!!! I just had my permanent crown placed yesterday and now all I can think is I have dead teeth- sponges that leave susceptible to this happening yet again. It’s been a trip. I currently have a rash on my cheek, chin and corner of my mouth. It was like chicken pox bumps. Itched and painful. ??? I was on a hefty course of antibiotics. Now I’m wondering.. who is still in there. Holistic Dentist! We are in process of moving and that will be one of the first things I look up once in Nevada – that and finding a doctor who can help me subdue Hashimoto’s. ♥️🧡🩷 Thank you SO much for taking the time to share your experience and what you e learned!💚invaluable! The feeling of not being alone!
Oh my, I am so glad that I came across this article. I was looking for something that could connect my thyroid neck pain to root canal pain and I struck gold. I had several root canals in my twenties with a host of other dental problems that led me to have crowns, filling, extractions, and a bridge Now that in my sixties I’m having pain in my head, neck and shoulder. The pain in my neck made me feel as if I had strep with increasing ear pain. Nevertheless, I was told that I needed a root canal on #2 tooth upper right. As a kid growing up in 1970 they used a lot of mercury and this one but now its covered with a bridge.. I was just going to have the root cannel but NOW I want the bridge out and the tooth pulled you just saved me thousands of dollars. I would love to save my teeth but at what cost
Have any of you been diagnosed with Graves? Sibo???? I have so many of these symptoms along with stomach issues for years. I was recently referred to an Endodontist for a tooth that has been having cold/heat sensitivity that had been previously repaired for a crack. I came upon this article and my mind is blown as it connects many of the issues that in my gut told me are interconnected?
Hi Karen, I have many Hypothyroid Mom followers who are hypothyroid post-treatment for Graves’ disease. Here are some helpful articles to read. I also offer individual consults if you wish to talk and receive helpful resources for your particular case: https://ny786.infusionsoft.app/app/orderForms/Talk-with-Dana-Trentini-30min
SIBO: https://hypothyroidmom.com/sibo-small-intestinal-bacterial-overgrowth-hypothyroidism/
GUT: https://hypothyroidmom.com/dysbiosis-and-thyroid-dysfunction-all-roads-lead-to-the-microbiome/
Good to have you at Hypothyroid Mom.
Hello, Hashi’s here as well! 1 root canal for 12 years now, still always hurting and swelling of gums. I’ve contemplated removal also, however I was wondering if you did any tooth replacement such as implant or bridge after?? I really don’t want an open space there as it is a major molar for chewing and would also be a gap when smiling! Thank you, Tasha
Knowing now the relationship between mouth and autoimmune diseases, it is a must to have a 3 D Cone Beam done asap!! I recommend to read the book HIDDEN EPIDEMIC written by Dr. Thomas Levy where he explains exactly what this article is all about.
Thanks for the book recommendation. I’ll be sure to read it. Good to have you at Hypothyroid Mom.
I have had dental issues for years multiple route canals and crowns you name it’s been done to my mouth. I was Diagnosed with Hashimoto’s disease about eight years ago and my thyroid antibodies yet to come down. Three years ago I had two root canals and within a week I went into a thyroid storm. At the time when I was going through the thyroid storm I never thought about the root canals but, once I got my body back to “normal “ I speculated I had something to do with the root canals.
I am currently facing having all of my teeth removed due to them just falling apart in my mouth. Call me Superficial but at my age I do not want to wear dentures. I am looking to get implants. No one can answer me on whether or not they are safe. Your article touches on it briefly but I was wonderingIf you have any further insight into implants
I felt like i was reading the story of my life!!!
I had a 2nd root canal to the same tooth last summer and this only made things worse!
Im finally getting that infected tooth extracted next week, after all these years of being really sick with all of your mentionned symptoms, i am really happy to see that hope is around the corner!!! I can hardly breathe and my left side of the body is problem after problem! Lost my thyroid, My B12 and iron are super low, i have a lot of heavy metals in my blood and tons of face/mouth swelling. I really hope to finally regain my health!!! Thank you so much for this article!!
I’m sorry to hear all you are going through Nicole. I’ve learned the hard way that an infected root canal tooth can wreak havoc on the entire body. There is hope to be well. All the best, Dana Trentini (aka Hypothyroid Mom)
I feel like I found my tribe… I’ve had so many root canals over the years. Now my thyroid has swollen.. also jaw and ear pain. seeing an endocrinologist tomorrow. So glad I found this site. I have been feeling there is a connection to all my symptoms. Wishing you all well!
Welcome to Hypothyroid Mom, June. Love having you on my site.
Hi June, Happy to have you on my site Hypothyroid Mom. Good to hear you are going to your doctor to check your thyroid.
I been hypnothroidmom for about 10 yrs or 12 yrs and I most depressed now then I was young
Hi Mary, It is good to have you at Hypothyroid Mom. I hope my site inspires you to get a second medical opinion for your thyroid.
This article is so relevant for me. I have Hashimoto’s and have had terrible jaw, tooth and ear pain. I had a root canal and it did not help at all. Of course, x-rays show nothing wrong. Just good to know that I am not alone.
Hi Donna, This is Dana Trentini from Hypothyroid Mom. Search your area for a dental office that has the panoramic x-ray that I mention in my article. I too had completely normal standard dental X-rays and it turned out that the infection was lower in my jaw below where the the standard X-rays capture.
Such an interesting article! I have soooo many root canals and extracted wisdom teeth. I am certain a lot of my health issues could be traced to my lifelong dental issues.
I am wondering if there was an alternative to extracting the root canal tooth, somehow clearing up the infection without extraction, because otherwise I might end up toothless!
Hi Hala, I wondered the same and went to multiple dentists including biological dentists for my own case which I share in my article. My case turned out to be a widespread type of infection based on the number and duration of my symptoms over time. My root canal was 25 years old by the time the infection was found so I felt in the end that extraction was my best option. Good to have you at Hypothyroid Mom.
You didn’t answer her question . I would like to know if any other alternatives before being toothless.
I just had an implant removed due to massive infection. All went well. No antibiotics. Felling weak and shaky on the third day after removal.
How long did it take for your hair loss to stop?
Similar to my problem .. both pain in the tooth and thyroid gland pains came together .. still after removing wisdom tooth after 2 weeks still all the neck and head pain s r there.. what shoud i do
Thank you for writing this, I suspect my tooth though not a root canal, has something to do with my inflammation. Did you do something to replace the empty space when you removed your tooth? If not have you noticed aay spacing happening between your teeth?
PLEASE tell us what you did to replace the extracted tooth!
I would like to know also plese
I need help I got a wisdom teeth removal 2 weeks ago. I can’t swallow, it hurts and I feel tired and my heart is working faster when I take or try to swallow food. I also had a root canal done in 2016, I always feel hot since 2016. Please contact me with more info. Email me.
I’m a male by the way
Is there something you can take not by prescription for hypothyroidism. My doctor dies blood work but never says anything and my symptoms of not able to swallow, goiter, hair loss, dry skin, bad teeth,brain fog, not able to concentrate and all the other multiple symptoms. I am tired of going to a doctor and paying and never having help. I’ve been told to pray and I’ve been told by doctor that I have to just get over it and that’s life. I would appreciate any advice!
See an endocrinologist and describe these symptoms.
What these people don’t say is that many, many dr’s, endocrinologist’s don’t really help at all. These articles are great and all but really doesn’t help with educating dr’s. We need to all get together on tv, etc. and have these dr’s to test for all thyroid problems, not just the norm. I literally had to tell my dr. To check t3, t4 etc. and they said NO don’t have too. Enough already
Dosi, I consulted multiple biological dentists in my case and I recommend the same to anyone that finds an infection in their tooth or jaw, as I had, to understand all your options before extracting a tooth.
I have had gunk and blood spurt out from the gumline under my lower right jaw root canal. Like you, I broke my teeth from grinding caused by malocclusion (which I finally addressed at age 50). The general contractor building our house has been a dental tech and he has suggested I investigate removal of it.
Since I had that done, I have been diagnosed with fibromyalgia, Reynauds. My dad and cousins have celiac but I developed allergies to almost every grain plus I have high a1c so haven’t eaten them intentionally since 2015. Rheumatologist dx me with leaky gut.
I am headed to a functional doc tomorrow to get tested for hypothyroidism as I have a preponderance of the symptoms on your long list.
May I ask how you addressed the replacement for the missing tooth?
Thanks for this article. What did you replace the extracted tooth with? Denture, bridge, implant? I’ve always thought my root canal was the contributing to my health problems, but like you have been told xray is ok. I’ve considered extracting it but I’m not sure what to replace it with.
I’d like to know also. I’ve been having horrible teeth problems too. Lost 2 in 1 week to breaks was going g to get implants but I just have been holding off.my jawbone is thinning so my dentist is pushing.
I was diagnosed of Chronic Obstructive Pulmonary Disease (COPD) in 2012 at the age of 63. I had been a heavy smoker, my symptoms started out with dry cough and shortness of breath, i ended up in the hospital, on a ventilator. I should have known it was coming, but like most smokers, thought it would never happen to me. My COPD got significantly worse and unbearable because of my difficulty catching breath. Last year, i started on a natural COPD Herbal therapy from Rich Herbal Gardens, i read a lot of positive reviews from patients who used the treatment and i immediately started on it. I had great relief with this herbal treatment. I breath very much better now, no case of shortness of breath or chest tightness since treatment. Visit Rich Herbal Gardens website ww w. richherbalgardens. com. This COPD treatment is a miracle, I feel better and breath better!!
Please answer if you had the tooth replaced or not. I am waiting to go to a biologic dentist and I want to have all the information at hand and whether or not you replaced or not was not confirmed in the article. I subscribe and read your articles faithfully, please help.
Four years ago I experienced a severe breathing problems. A year later, it worsened and I was diagnosed of COPD. I came across Herbal HealthPoint (ww w. herbalhealthpoint. c om) December, 2018 and learnt about their successful herbal therapy for COPD. I immediately started on the COPD treatment; i began to notice a reduction in symptoms till it all vanished. I feel better and breath better. I Just wanted to share for people suffering from this horrible lungs disease.
I had a root canal done in my eye tooth 🙁 My Hashimotos dx came 2 years after my root canal. I dont have any pain with it but I cant imagine getting it removed because it’s in my smile line……. :(:(:(:( any thoughts??
HI, this is all so interesting to me. I had a total thyroidectomy due to cancer. After receiving the radioactive iodide tablets for my scans I started having trouble with my salivary glands and tear ducts, which my doctor said was common also. However I have had lots of dental work since this surgery multiple extractions, pain where there is no cavities, also great sensitivity due to the enamel decreasing on my teeth, none of this happened until after my thyroid removal and treatment. I have had problems with jaw pain due to the salivary glands but I never thought that maybe my sinus and dental issues I deal with now could relate. Thanks for sharing everyone.
I didn’t have any major problems with my salivary glands after RAI, but it did reduce the saliva flow. I sure that is has contributed to my already poor teeth. And then medications (anti-depressant) that causes dry mouth. Biotene products are designed for dry mouth issues. I get painful salivary gland swelling (chipmunk cheeks) if I let myself get dehydrated during hot weather.
This is a very timely issue for me. I’ve had issues with an upper left jaw root canal. It has been going on for a year. I’m scheduled to have the root removed in Nov. This past year I’ve been having a lot of inflamation and have been diagnosed with sclerosing mesenteritis. Maybe having this root extracted will make a difference. Did you have tooth replaced? My dentist is recommending an implant.
I had a severely infected root canal. I had flu like symptoms for over a year,, jaw pain and a knot on my jaw. I do feel so what better. I recently went to my Dr. and there was still some of the broken tooth in the site. I’m trying to figure out what to do. You did not replace the tooth?
I had a severely infected root canal. I had flu like symptoms for over a year,, jaw pain and a knot on my jaw. I do feel so what better. I recently went to my Dr. and there was still some of the broken tooth in the site. I’m trying to figure out what to do. You did not replace the tooth?
This is incredibly interesting! I was diagnosed with Hashimoto’s and then had 2 root canals some years later. I have several of the symptoms mentioned in this article, including sporadic recurring tooth pain in the teeth that had root canals. Regular dental x-rays always show nothing. This article also has more than a few typos. I would be happy to help with this!