
Most conventional doctors rely on TSH as the gold standard to measure thyroid functioning. Many mainstream doctors do not run a full thyroid panel that should at least include Free T4, Free T3, Reverse T3, and thyroid antibodies. Unfortunately TSH alone does not provide a complete picture. If doctors are going to rely on TSH alone, however, they should at least give consideration to the controversy over the TSH normal reference range and consider this when diagnosing patients. Right? We are more than a lab number. It’s up to us to take control of our thyroid health and insist our doctors treat us the patient and not this controversial TSH lab number, even if they look at us like we are CRAZY for questioning them!
The thyroid gland is a little butterfly-shaped gland at the base of our necks. TSH stands for Thyroid Stimulating Hormone, a hormone produced in the pituitary gland in the brain that tells the thyroid how much thyroid hormone to make.
Typically, if there is a low level of thyroid hormone in the body, the pituitary will increase production of TSH to stimulate the thyroid to produce more thyroid hormone. Therefore a high TSH level suggests an underactive thyroid (hypothyroidism), while a low TSH indicates too much thyroid hormone in the body (hyperthyroidism).
In my post “Miscarriage in New York City…Be Thyroid Aware”, I outlined the TSH ranges for pregnancy and provided trimester-specific ranges. In this post I would like to discuss the normal TSH lab standards for non-pregnant adults.
Thyroid Stimulating Hormone
For many years, most mainstream doctors have considered TSH level >10 mIU/L evidence of overt thyroid failure, and levels of 5-10 mIU/L evidence of mild or subclinical hypothyroidism. Many doctors refuse to treat hypothyroidism if a person’s TSH is less than 5 mIU/L even when the patient presents with classic hypothyroidism symptoms. This strict reliance on 5 mIU/L has left many hypothyroid people suffering with debilitating symptoms and yet their doctors refuse treatment.
For over a decade there has been considerable debate about the correct upper limit of the reference interval for TSH. According to the old standards 5.0 mIU/L is the upper limit. This upper number is critical in determining who is diagnosed with hypothyroidism and who is not.
Modern medicine continues to argue within itself on the proper upper limit of the reference range for TSH.
One of the largest studies of thyroid problems in a population is the Whickham Survey, which studied the thyroid levels of 2,779 randomly selected adults living in the town of Wickham in England from 1972-1973 and subsequently followed for 20 years. Data from the twenty-year follow-up published in 1995 demonstrated an increased risk for the development of hypothyroidism once TSH exceeds 2.0 mIU/L.[1]
The third National Health and Nutrition Examination Survey (NHANES III) screened 17,353 subjects from 1988 to 1994 and excluded those with diseases or factors known to affect thyroid function. In the resultant ‘normal’ population of 13,344 subjects, 95% had TSH levels that fell between 0.3 and 2.5 mIU/L.[2,3]
These findings supported the establishment of a narrower TSH reference range and a lowering of the upper limit of the range.
The National Academy of Clinical Biochemistry (NACB) in 2002 recommended that the upper limit of the reference range be lowered:[4]
The recent follow-up study of the Whickham cohort has found that individuals with a serum TSH >2.0 mIU/L at their primary evaluation had an increased odds ratio of developing hypothyroidism over the next 20 years, especially if thyroid antibodies were elevated.
In future it is likely that the upper limit of the serum TSH reference range will be reduced to 2.5 mIU/L.
In 2003, the American Association of Clinical Endocrinologists issued a press release in support of lowering the upper limit of the reference range:[5]
Until November 2002, doctors had relied on a normal TSH level ranging from 0.5 to 5.0 to diagnose and treat patients with a thyroid disorder who tested outside the boundaries of that range. Now AACE encourages doctors to consider treatment for patients who test outside the boundaries of a narrower margin based on a target TSH level of 0.3 to 3.0. AACE believes the new range will result in proper diagnosis for millions of Americans who suffer from a mild thyroid disorder, but have gone untreated until now.
However in 2012, the Clinical Practice Guidelines for Hypothyroidism in Adults: Cosponsored by the American Association Of Clinical Endocrinologists and the American Thyroid Association recommended 4.12 as the upper limit of normal for TSH.[6] (Wait! What happened to the AACE’s press release in 2003 to reset the TSH level to 0.3 to 3.0? Do you see the craziness of all this?)
Thyroid Advocacy To Lower The Upper Limit of TSH
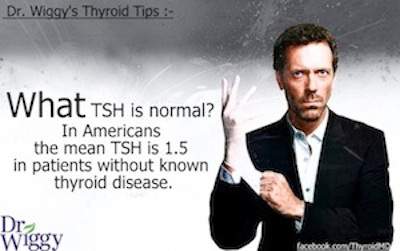
Thyroid advocates and many integrative physicians are fighting to narrow that range. Thyroid doctor Dr. Weston “Wiggy” Saunders posted this important message:
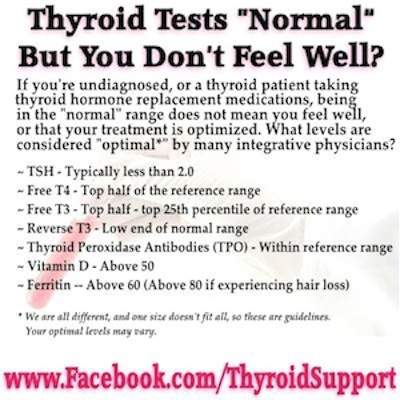
Thyroid advocate Mary Shomon, from Very Well Health Thyroid Disease, shared this important list of recommended lab tests and optimal ranges. Note the optimal TSH range listed.
When I was initially diagnosed with hypothyroidism after the birth of my first son in 2006, I listened to my doctors unquestioningly. I assumed that my doctors were the experts and that they knew everything there was to know about this disease. My doctor was using the old 0.5 to 5.0 TSH lab standard and kept telling me my TSH was normal falling in this range, yet I felt awful. Under my doctor’s care my TSH levels rose to 10.0 mIU/L.
At a TSH of 4.0 I felt sick and tired. By the time my TSH rose to 10.0, I felt like the walking dead struggling to make it through each day.
I even had one doctor who said she only treated a person for hypothyroidism when their TSH rose above 10.0 otherwise it was unnecessary. WHAT?!! I couldn’t function at a TSH of 10. I couldn’t get up from my bed to take care of my young son.
What Should You Do?
What if you have many symptoms of hypothyroidism, but your doctor is testing TSH only and your TSH is “normal”. What should you do?
What if you are being treated for hypothyroidism but you still suffer symptoms and your doctor is insisting your treatment is fine because your TSH is “normal”. What should you do?
Don’t just accept “your thyroid is normal” from your doctor. Insist on a full thyroid panel not just TSH but also Free T4, Free T3, Reverse T3 and thyroid antibodies. Get a copy of your lab results and check your scores yourself, even if your doctor acts like you are crazy (because you are NOT)!
I’m thankful that I found a great doctor who understands that I am more than my lab numbers. My doctor listens to me and my symptoms and for this I am grateful. TSH is only a number and it doesn’t give an accurate picture of my thyroid health. There are people like me on thyroid medication who feel our best when our TSH is below the ‘normal’ range. I feel fabulous with a suppressed TSH without signs of over-medication.
If I had a doctor that looked at TSH alone, I would be a very ill woman today.
If your doctor won’t do the additional tests and insists on relying on TSH while you suffer symptoms, find a new doctor. Find a doctor who understands you are more than a lab number. There are good thyroid doctors out there.
Do NOT settle.
References:
1. Vanderpump, M.P., Tunbridge, W.M., French, J.M., Appleton, D., Bates, D., Clark, F., Grimley Evans, J., Hasan, D.M., Rodgers, H., Tunbridge, F. The incidence of thyroid disorders in the community: a twenty-year follow-up of the Wickham Survey. Clin Endocrinol (Oxf) 1995 Jul;43(1): 55-68.
2. . Hollowell, J.G., Staehling, N.W., Flanders, W.D., Hannon, W.H., Gunter, E.W., Spencer, C.A., Braverman, L.E. Serum TSH, T4, and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 2002 Feb;87(2):489-99
3. Lee, S.L. When is the TSH normal? New Criteria for diagnosis and management.. Lecture presented at 12th Annual Meeting of the American Association of Clinical Endocrinologists (AACE), San Diego, CA, May 14, 2003 (thyroidtoday.com)
4. National Academy of Clinical Biochemistry 2002. Laboratory Medicine Practice Guidelines: Laboratory Support for the Diagnosis and Monitoring of Thyroid Disease. Retrieved from: http://www.aacc.org/sitecollectiondocuments/nacb/lmpg/thyroid/thyroid-fullversion.pdf
5. American Association of Clinical Endocrinologists (January 2003 Press Release). Over 13 Million Americans with Thyroid Diseases Remain Undiagnosed. Retrieved from: www.hospitalsoup.com/public/AACEPress_release-highlighted.pdf
6. . Clinical Practice Guidelines for Hypothyroidism in Adults: Cosponsored by the American Association Of Clinical Endocrinologists and the American Thyroid Association. Retrieved from: https://www/aace.com/files/hypothyroidism_guidelines.pdf

This is all fascinating. I decided to unravel it from a different far distant shore. Abram Hoffer and his book on oxidized stress hormones like adrenaline and adrenochrome. The primary chemical and the secondary, and the 2nd having anti-thyroid properties drew me into the thyroid stimulating hormone maze! Now I am trying to fathom the big picture on what is happening on a deeper,more complex level. It the early stages of biochemical inbalance,the human is unaware something chemically sinister is conspiring in the body. If it is not remedied,the results seem infinite, intra-reactionary and impacting. Human says only, ‘ I don’t feel well’, and the doctor,well lately your gambling at the casino of life. Its all so very complex, but there are good doctors and correct hypothesis explaining clearly the basic conversion process,but leaving, but important key evidence results in a mistaken overall picture with half truth and partial to murky vagueness. Fill in the blanks. Patient Heal Thyself. Easier said than done depending on how long the damage has been done.
I have felt awful for several years. My primary doctor only goes by TSH. Mine has ranged from 3 to4. My hair is falling out, nails are brittle, dry skin, use to be hot, now always cold, in a fog, treated for depression, and incredibly fatigued. I finally went to an endo and was told my tests were normal, isn’t that great? My results may be in the old range but not in the functioning, or optimal range. Yay, my tests are called normal, but I feel sicker and sicker! Can anyone else relate??
Also, I forgot to say an ultrasound on my thyroid shows inflammation!
Hi, I have been trying to figure if my numbers are at an optimal range. I feel my endo is not concerned about my plethora of symptoms.
I have been feeling like I’m trapped in my own body for a while. I suffer from constant mood changes, irritability, hair loss, weight gain and loss, irregular periods, heart palpitations, extreme anxiety and vision loss( I was diagnosed with chronic dry eyes and in almost blind in one eye. I have bad circulation and tingling and numbness in my fingers, suffer with dizziness and vertigo often and lightheaded
This are my quest diagnostics labs
TSI 143
T3 free 2.8
T4 free 1.3
THYROID PEROXIDASE ANTIBODIES<1
FSH 3.3
T4 (THYROXINE), TOTAL 8.6
ESTRADIOL 40
VItamin D 45
TSH 0.87
LH 3.3
PROLACTIN 14.7
Estrone lc/ms/ms 51
Estriol serum <0.10
Testosterone total 20
Testosterone free 1.6
I hope someone can provide some assistance. I'm in the process of finding another endo.
I have Hashimoto’s disease. If your TSH is under 1 that’s phenomenal I hit around 5 on my meds feel fine. If your first being treated your doctor would have you come in multiple times as its statistically pretty much impossible that you have it especially if you’re “exhibiting” symptoms. These symptoms are generally shared amongst many diseases both known and unknown. In your case it’s not likely hypothyroidism, if you had it you’d be too brain fogged to notice the symptoms. It’s actually a problem of people with this disease to stop treatment because they feel “fine” even when unable to do tasks they normally do.
I for example an engineer may feel good but I’m usually not paying attention to the fact I can’t do math without a calculator.
Given your symptoms and noticing you omitted or didn’t get it checked what’s your blood glucose level? I also have type 2 diabetes and those share a lot of those symptoms
Dear Mom, My tsh was 0.01 on 175mcg levo, and I felt great. My tsh is now 0.01mcg on 150mcg levo, and I have many hypo symptoms and feel***. Have you heard of other cases where the patient had hyper test results with hypo symptoms? Thank you in advance for your assistance. Walt
Hi Walter, Yes I hear from Hypothyroid Mom followers that have suppressed TSH (below normal) and feel great without symptoms of overmedication like rapid heartbeat, tremors, insomnia, shaking, rapid weight loss, etc. This is the case for me where I feel my best when my Free T3 is top quarter of the normal range but my TSH is low like yours but I feel great. This can be confusing for doctors that only look at TSH, especially for those of us on T3 medications like natural desiccated thyroid. Here’s an article about this on my site:
https://hypothyroidmom.com/tsh-wars-the-unreliable-thyroid-lab-test/
good afternoon everyone, i feel everyone’s frustration. I havent felt the same since i had my thyroid removed ten years ago. if your doctors are not giving you concrete answers of help find someone else. i seen several endos and all of them were like “no it doesnt have anything to do with your thyroid condition.” which is bullshit…….. I started researching and self helping myself. The aching of my joints, low libido, dry hair, tiredness, etc. I started taking sea kelp and selenium everyday, and the aching joints and fatigue is much better. The only thing that i was told to take was the Vit D. No doctor recommended the iodine. i was running from this doctor to that doctor thinking that it was other issues going on when it wasnt. I see a new doctor on june 12 and im asking for a full blood workup. if the doctor is not willing to treat and teach you about your condition, find someone that will and try to help yourself. change your diet and exercise. read about supplements. my issue right now is heart palpatations and acid reflux which i know has come from the thyroid issue. my meds might need to be changed….. when all in doubt go get your TSH checked asap.
I am diagnosed with hashimoto’s disease. The symptoms you’re complaining about are common with a large range of diseases. The difference between you and me is altering my T4 levels will help me because I have the disease. I’m sincerely sorry if you’re suffering from an unspecified disease but if your thyroid has normal TSH T4 and T3 it’s not a thyroid problem. My levels without meds is an easy 13 and I get such a brain fog I don’t notice how poorly I’m doing, give me 125mcg and I’m fine again. If they give you T4 with normal levels that would just give you hyperthyroidism
Normal TSH, T 3, T4? The parameters for “normal “ are quite wide. Many, many years ago a very good and perceptive doctor ( Gyn) told me I had a thyroid problem. My PCP ignored this doctor and told me I was just depressed and refused the antibody test for Hashimotos.. ( I had read about). Went to new doctor who agreed to antibodies test and found I was in the thousands. Eventually had thyca. There is nothing necessarily ”normal“ about thyroid labs just because they’re within “normal” parameters. That’s one of the big problems with the TSH Reflex test that appears to be used more and more by non-Endocrinologists.
I would recommend to everyone: Look online for Dr. Amy Myers and Dr. Izabella Wentz, they are thyroid gurus. Also try the paleo diet, it will probably help.
I just went to my doctor and he didn’t see me but, his assistant seen me. She said my T4 -1.68 was to high and reduced my Synthroid I was on 88Mcg. she reduced it to 75Mcg and they called and said everything was okay I got a copy of my lab report and see that my TSH is high its 4.73 now I’m feeling tired and my hair is looking brittle worried that some thing is going on. now my T4 is 2.5 should I be on a high dosage, thinking of changing doctors.
Hi Emily, You’ll find a chart of optimal ranges for lab tests in this article that I wrote. Get a second opinion. I felt awful at a TSH of 4 like yours.
https://hypothyroidmom.com/top-5-reasons-doctors-fail-to-diagnose-hypothyroidism/
Hi!
I just got my lab results back. They want to decrease my ArmourThyroid. I am currently on 135 mcg and they want me to drop 15 mcg due to my T3 being to high – 2.78.
My results are as follows:
TSH- .28
T4- 1.57
T3- 2.78
I always get concerned when they want me to decrease my meds. I’m really trying to get them to run the complete Thyroid panel. I see an endocrinologist in Baltimore, I would to find an endocrinologist that works with just your thyroid.
Thanks and have a fabulous day!
I have family members with thyroid issues, have many of the symptoms, but my regular doctor just tells me my labs are normal. I’ve seen conflicting levels of normal levels while researching. Can anyone tell me what normal levels should be for a 33 year old woman?
My TSH is 0.06 with Free T4 1.2 that is all my doctor will test. I do not have a thyroid gland. I take 100 mcg Synthroid 15 mcgs Cytomel but am cold, can’t lose weight, diabetic, fatigue, low Basel body temperature, etc. My doctor wants to reduce my meds! What do I do?
You need a new doctor for sure. Vitamin D is important. Get all labs done.
Thanks for posting ur experience. Mine is 5.2 and they want me to take that xact dose! The reckless doctors at the VA didn’t even listen to me. I am reluctant to suffer your dilemma as I believe there r many factors especially Stress and life style change. I also see this was my reading in 2011! Obviously more complex testing or gradually stopping the meds if they are harming u!
My tsh came back 3.5 with a borderline ldl of 138. I am 35, 5 feet tall 133 lbs and all the weight on my stomach. I am constipated all the times, cold when everyone else seems fine, losing hair and have gained weight in last year and regardless of how healthy i eat and how much I exercise it doesn’t change. I am also irritated all the time. I am pretty sure my doctor will say it’s normal as when i told her i want to get my thyriod checked she said well if its not thyriod we have to work on your diet. I am sick of eating nothing and worrying about my weight all the time.
I am a 65 yr old female and I was diagnosed 6 months ago with hypothyroid. I was given 25mg levothyroxine at first and later increased to 50mg. In 6 months I put on over a stone and a half in weight and my joints ached unbearably, diff sleeping, hot and cold flushes, headaches and tiredness continually. I stopped taking my thyroid tabs had another blood test and there was no difference in the reading. So taking the tabs and weight increase ++ was all for nothing! My reading was/is TSH 5.37. I cannot bear the thought of staying on the tabs and getting even fatter and not sleeping etc. Any advices would be greatly appreciated. Thanks, Katy
This reply is late compared to when you posted. But I just saw your comment. Levothyroxine did not work well for me. I had to ask my Dr to switch me to Synthroid the brand name. I am on Synthroid 100 mcg. I have been Hypo for over 3 years now. Synthroid has helped all my symptoms go away and helped me lose the belly fat, not feel so fatigued and my hair stopped falling out. If anything, the right medication at the right dose will help all your symptoms. There are very little side effects from these medications that I have experienced. I would go back to the doctor and have them adjust your dosage to get it to the right dose. I am a 38 y/o female.
Please inform me by email can i eat seaweed everday
regards
[email protected]
Hi There,
I just got these labs from my endocrinologist and I wanted a different perspective on them.
Can you tell me your thoughts?
I am a 47 year old Lebanese female who is “5” ‘4 3/4″ and weighs 169 lbs. I have lost 46 lbs since last December 19, 2015.
I have PCOS and genetically inherited high cholesterol and high blood sugar. Besides genetics I am a sugar addict and have binge eating disorder.
I have been pre diabetic off and on for at least 5 years. I have never been diagnosed with diabetes as I have never reached diabetic numbers through a self induced OGTT, A1c tests, fructosamine and fasting blood sugars.
I am working on my diet and exercise to reduce certain blood markers.
My blood sugar has come down and I am still working on my cholesterol. The cholesterol was measured by my primary care doctor and cardiologist.
The blood work below was from last week at my Endocrinologists office.
My last total cholesterol was 360 but my hdl and triglycerides were in normal range. Taken about a couple months ago.
Last spring my total cholesterol was 259 coming down from 312. Prior to 312 it was 344.
When it was 259 my hdl and trigs had also improved.
I think it went high again because I started eating sugar again. I was still losing weight and monitoring my caloric intake but I went Paleo almost sugar free from December 2015 to April 2016 and that’s when my cholesterol came down from 312 to 259.
I am back to minimizing sugar intake.
I also suffer from depression, anxiety and ocd.
I started gaining weight when I hit puberty and developed PCOS. I have lost and gained weight many times since then.
I carry most of my weight in my belly.
I am having a hyperoscopy done on Dec 15. Some hyperplasia was found in my uterus.
I have never had kids. My period has been regular since my early thirties.
Please let me know if you need any more information.
I appreciate your insight!!
Thank you very much.
Sincerely,
Vivian
T4, FREE, NON-DIALYSIS: 0.9
T3, Free: 2.6
TSH: 2.33
THYROGLOBULIN ANTIBODIES <1
THYROID PEROXIDASE ANTIBODIES <1
Fructosamine: 243
A1C: 5.4
TESTOSTERONE,TOTAL,LCMSMS: 20
TESTOSTERONE, FREE: 2.7
Insulin: 3.8
DHEA SULFATE: 62
C-PEPTIDE: 1.31
Vitamin D: 25
SODIUM 137
POTASSIUM 4.2
CHLORIDE 103
CARBON DIOXIDE 27
GLUCOSE 92
UREA NITROGEN 10
CREATININE 0.71
BUN/CREATININE RATIO N/A
Bun/Creatinine ratio is not reported when the BUN
and creatinine values are within normal limits.
CALCIUM 9.9
PROTEIN, TOTAL 7.1
ALBUMIN 4.2
GLOBULIN, CALCULATED 2.9
A/G RATIO 1.4 1
BILIRUBIN, TOTAL 0.4
AST 12
ALT 13
ALKALINE PHOSPHATASE 40
Fasting reference interval
NON-AFRICAN AMERICAN EGFR 101
My tsh goes from 3.5-3.8. I feel so tired. My joints hurt. My belly is getting bigger but my arms and legs stay super small. Absolutely no sex drive. I feel depressed. And am actually getting treated for depression. I am a male in 30s. I have paternal grandmother with hypothyroidism. Would levo help me feel normal. I need help I’m just so lazy and tired feeling and moody I feel like I’m a horrible dad…single dad.
Hi Thomas,
So sorry to hear about this, I had the same problem. My doctor did reluctantly put me on Levo when I got to 3.9 although it really didn’t work for me. After reading through a lot of websites and doing my own research, I found out about Thyrogold (on sttm) and I decided to stop taking the Levo and give it a try. I am still trying to find the correct dose as I went to the doctor yesterday and my TSH is currently .01 which is too low. I do feel amazing and I’m not having a hard time sleeping or anything, if my test results would not have been low I would have thought I was in a normal range. When I decided to look into getting Natural Dessicated Thyroid on my own was the last time I saw the doctor in July my blood pressure was 86/49 and my heart rate was 49, they wouldn’t let me leave before giving me an EKG. Not to mention I felt horribly tired from morning until night and just overall terrible. Hope all works out well for you