Have you had saliva cortisol testing done? I have and it was one of the most important pieces to my thyroid puzzle. Turned out my cortisol was low throughout the day.
Written by Cammi Balleck, CTN, ANCB Board Certified Naturopath
Where is your cortisol level?
Do you know that excess cortisol can be the CAUSE of:
- decreased metabolism
- depression
- high blood pressure
- chronic fatigue
- insomnia
- migraines
- tunnel vision
- acid reflux
- hostility
- hunger
- arthritis
- low immune system
CORTISOL is an important hormone in the body, secreted by the adrenal glands and involved in the following functions and more:
- Proper glucose
- Regulation of blood pressure
- Insulin release for blood sugar maintanence
- Immune function
- Inflammatory response
Did you know cortisol lowers your thyroid hormones?
Here is the simple truth:
Stress triggers the adrenal hormone cortisol.
Cortisol triggers the flight or fight response.
Over time cortisol lowers thyroid hormones.
Ok so here is the dirty truth, this is why weight loss is so hard with hypothyroidism, not only is your thyroid function low, but your cortisol being high slows down weight loss and on top of that cortisol causes your thyroid to work even slower. In addition to negative effects of cortisol like increased blood sugar, high blood pressure, poor digestion, poor immune function, it also lowers thyroid hormones. When the body is pushed too hard, thyroid hormone and the metabolic rate goes down. This is the body’s way of protecting itself, like pushing on the brakes in a car that’s speeding down a hill. It’s a fact cortisol messes with your thyroid hormones.
1. Cortisol decreases TSH, lowering thyroid hormone production.
2. Cortisol inhibits the conversion of T4 to active T3, and increases the conversion of T4 to reverse T3.
The other most significant indirect effect the adrenals have on thyroid function is via their influence on blood sugar. High or low cortisol can cause hypoglycemica, hyperglycemia or both. Blood sugar imbalances cause hypothyroid symptoms in a variety of ways.
Always remember adrenal stress also has a more direct impact on thyroid function. In order for thyroid hormone circulating in blood to have a physiological effect, it must first activate receptors on cells. Inflammatory cytokines have been shown to cause hypothyroidism.
If you’re familiar with insulin resistance, where the cells gradually lose their sensitivity to insulin, this is a similar pattern. It’s as if the thyroid hormone is knocking on the cell’s door, but the cells don’t answer. A perfect example of this in practice is the Hashimoto’s patient who is taking replacement hormones but still suffers from hypothyroid symptoms – often in spite of repeated changes in the dose and type of medication. In these patients, inflammation is depressing thyroid receptor site sensitivity and producing hypothyroid symptoms, even though lab markers like TSH, T4 and T3 may be normal.
Who isn’t stressed these days?
On top of not feeling good, you have kids to take care of, dinner to make, parents to help, deadlines to meet, traffic, bills, illness, anger, phone calls, and family. We either exercise not enough or too much. Most people can admit to eating foods that are not ideal and when we are tired and stressed we stop for a fancy coffee and sweet bite to feed our flesh because it’s been a long day. This stress is not just one day – it is long term, day after day after day.
What happens if long term stress continues?
If the adrenals are put under stress long enough, they eventually become exhausted. At this point, the adrenals won’t even be able to make a normal amount of cortisol.
The two conditions of hypothyroid and hypoadrenal are hand in hand friends and often come together. I believe in order to feel better instead of thinking in terms of just hypothyroidism, it is wise to think in terms of a hypo-endocrine system.
Cortisol is one of the hormones released by the adrenals during the stress response. Prolonged cortisol elevations, caused by chronic stress, decrease the liver’s ability to clear excess estrogens from the blood. Excess estrogen increases levels of thyroid TBG, the proteins that thyroid hormone is attached to as it’s transported through the body.
When thyroid hormone is bound to TBG, it is inactive. It must be cleaved from TBG to become “free-fraction” before it can activate cellular receptors. (These free-fraction thyroid hormones are represented on lab tests as “free T4 [FT4]” and “free T3 [FT3]”.)
When TBG levels are high, the percentage of free thyroid hormones drops. This shows up on labs as low free T4/T3.
If you are hypothyroid I highly recommend you look at your body as a whole and you know where your cortisol is as well as your thryoid hormones.
Normally, cortisol is present in the body at higher levels in the morning and at its lowest at night.
Although stress isn’t the only reason that cortisol is secreted into the bloodstream, it has been termed “the stress hormone” because it’s also secreted in higher levels during the body’s fight or flight response to stress, and is responsible for several stress-related changes in the body. Small increases of cortisol have some positive effects:
- A quick burst of energy for survival reasons
- Heightened memory function
- A burst of increased immunity
- Lower sensitivity to pain
- Maintenance of homeostasis in the body
While cortisol is an important and helpful part of the body’s response to stress, it’s important that the body relaxes so the body’s functions can return to normal following a stressful event. If you are not sleeping it could be your cortisol. Unfortunately, in our current high-stress culture, the body’s stress response is activated so often that the body doesn’t always have a chance to return to normal, resulting in a state of excessive stress.
Higher and more prolonged levels of cortisol in the bloodstream like those associated with chronic stress have been shown to have negative effects, such as:
- Impaired cognitive performance
- Suppressed thyroid function
- Blood sugar imbalances such as hyperglycemia
- Decreased bone density
- Decreased muscle tissue
- Higher blood pressure
- Lowered inflammatory responses in the body and other health consequences
- Increased abdominal fat, which is associated with a greater amount of health problems than fat deposited in other areas of the body
To keep cortisol healthy and under control, the body’s relaxation response should be activated after the fight or flight response occurs.
Cortisol is normally 10 times higher in the morning than at night. However, in adrenal dysfuntion (either too low or too high cortisol) there is also a change in this basic pattern of cortisol release. As covered in the charts below, there is simply no way to accurately guess cortisol levels at 8PM based on a single 8AM sample.
Therefore, multiple cortisol samples are needed throughout the day. If testing blood, this would require multiple blood draws during the same day, which is just simply not practical.
Waking up extra early in the morning to run to a lab and get stuck with a needle is a big stress in itself and may alter the level of the body’s main stress hormone cortisol. Therefore, this is testing cortisol levels when a patient is under unusual levels of stress in the morning, not during a typical day.
Saliva tests require people to merely spit in a tube. This is a much less stressful test than getting a blood draw, and so getting the test itself will not change cortisol levels.
The saliva cortisol test
Saliva cortisol is usually measured 4 times during the day: upon waking up, noon, the late afternoon and before bed. Saliva is collected by spitting into a small collection tube, therefore it can be collected just about any time or any place. This is often referred to as an ASI or Adrenal Stress Index test.
Adrenal Stress Panel is used when individuals are complaining of:
- fatigue
- weakness
- insomnia
- headaches
- irritability
- nervousness
- sugar cravings
- dizzy spells
- decreased stamina
All individuals with chronic disease will have changes/compromises in their adrenal function.
Cortisol Patterns
It is never good sense to “guess” whether you have high or low cortisol, even if you “think” you do! Symptoms of high cortisol can be similar to symptoms of low cortisol. Plus there are different variations of an adrenal problem which require different supplements.
The following examples show why cortisol needs to be measured throughout the day and the usefulness of this information.
Reference range is highlighted in green. Either too high, or too low cortisol is not a good thing.
Low cortisol, adrenal fatigue results
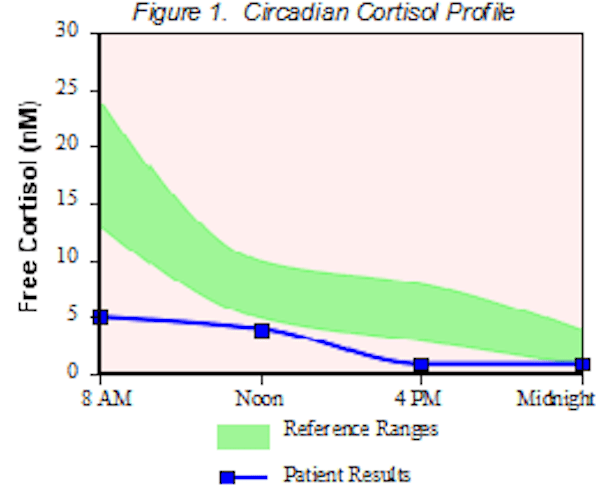
In this case cortisol is low through the entire day. Simply taking some herbs like adrenal adaptogenic herbs and B vitamins (common advice for adrenal fatigue) would not nearly be enough support for someone in this situation.
In addition comprehensive health history would need to be reviewed, as this sort of adrenal fatigue doesn’t just happen for no reason. Major stresses (psychological or from other illnesses) need to be dealt with in order to relieve some of the stress on the adrenal glands.
High and low cortisol, cortisol deregulation
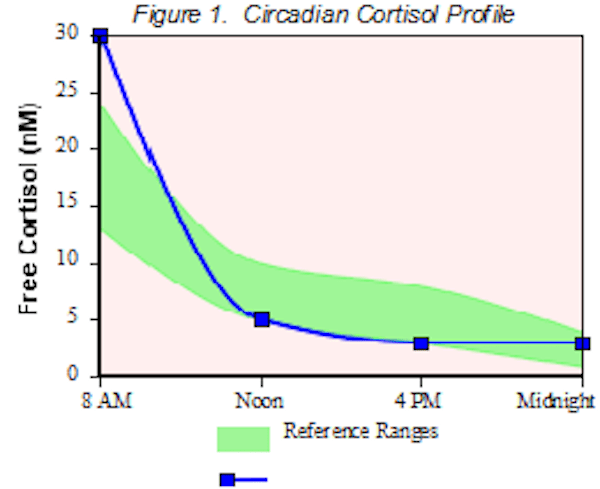
Morning cortisol was so high it was literally off the chart. For the rest of the day it followed at the very bottom of reference range.
Such high AM cortisol indicates how the stress response may be causing insomnia, such as waking up 3AM or 4AM every night.
This person may respond better to supplements that help the brain better regulate cortisol production (which is controlled by the hypothalamus and pituitary glands) than taking boat loads of adrenal supplements for daytime fatigue. This person would also be helped with minerals.
Phosphatidylserine is a well-known cortisol suppressor used in the evening. Some other OTC nutritional supplements to lower cortisol levels in the body include Zinc and acetyl l-carnitine.
More patterns of cortisol deregulation


In these two cases rising cortisol during the end of the day (when cortisol should be decreasing) shows cortisol contributing to inability to fall asleep.
In the first case morning fatigue related to low cortisol can be seen. The increase in cortsol was related to blood sugar imbalance (besides energy production, cortisol works very closely with insulin to regulate blood sugar), so nutritional support for both the adrenals and blood sugar was needed.
I recommend a low-glycemic diet balanced in protein, healthy fats, and complex carbohydrates like vegetables, eaten as smaller meals more frequently (5-6 small meals/day), has a positive influence on hormones. Protein is important for the adrenals and requires adequate stomach acid (HCL) for digestion.
The second case has a large drop between 8AM and Noon, which indicates stress coming from the gastrointestinal system which must also be treated. This person would need probiotics![]() and GI support
and GI support![]() .
.
About Cammi Balleck
Cammi Balleck is an ANCB Board Certified Traditional Naturopath. She has been called the leading Happy Hormone Doctor. She has over 11 years experience specializing in biochemical balance and she is author of the book Happy the NEW Sexy. Cammi is the women’s health expert for Women’s Day, O, Prevention, Shape, and First Magazines as well as a featured expert for TBN, and FOX NEWS NATIONALLY. In addition she has made guest appearances on CW stations in Denver.
Thanks for this excellent article-I found it very useful.
I myself have a cortisol profile very similar to the last profile shown here-a sharp drop off in cortisol. I’m fascinated about the idea the this sharp drop off indicates gastrointestinal issues-are there any references to this? Is this always the case when a sharp drop off is seen like this in the AM? I’m trying to get to the bottom of this but any practitioner I’ve worked with so far has not mentioned this link to GI issues and cortisol. Is there anywhere I can find more info on this or any one I can work with who understands this? Thanks very much, Dee
Hello – thank you for sharing your knowledge with us. I have hypothyroidism & just had a saliva cortisol test, which showed very low (below the range) morning cortisol, & very high (well above the range) for the rest of the day. (4 time saliva trst.) my thyroid labs were recently worse & medicine has been adjusted, but even when numbers looked better I still struggled with hypothyroid symptoms at times, as well as feeling as if I would faint, especially when standing up, but also related to heat & stress. Have you ever heard of something like this, & do you know how I can treat the low morning cortisol & high afternoon evening cortisol? If I understand correctly, the cortisol issues could be preventing the thyroid hormones from reaching the cells as well. Thank you for any information you might have.
Your article has no references, which would make it more credible. I would love to cite your article but your lack of references makes it difficult to do so.
Hi there Thankyou so much for the article ! I live in Australia and have been diagnosed with hashimotos.. so you think you could explain why my acne would clear while being hypothyroid it cleared just before hashimtos diagnosis
Thanks so much
Very interesting post-alot is my life last 29 yrs and sick of stupid mental health diagnosis that don’t fit my symptoms at all,just to be fobbed off with cheap ineffective meds!
Have had what i think were simple partial seizures(not diagnosed as only med treated mental health is here!)since 1989. This caused fight or flight/high cortisol(and broken sleep!)which also caused hypothyroid symptoms since 91(diagnosed in 2004). Now at stage where on crappy t4,have diagnosed high cortisol,awaiting possible Cushings Disease(pituitary tumour) to be outright poo pooed. Can’t have high ACTH/Cortisol and low thyroid hormones-right?
I have PTSD and now my SSRI’S are not working properly, The doctor put me on prozac, and my morning anxiety is through the roof. I had morning anxiety about 6 months ago, without any medications, and started taking adrenal health (adaptagins). After starting the adaptagins the morning anxiety went away. I have a nodule on my thyroid, T3 and T4 cells came back normal, so primary doctor is not worried about it. I went to mental health this morning to see what to do because of the severity of the morning anxiety, I asked for a cortisol test and the doctor looked at me funny and put me on antipsychotics. Is this the answer? I am also in menopausal stage. I feel like a nut case, and am scrambling on what to do. I know my body, I know me and I know something is not right. I am stopping the prozac but unsure if I want to start Ambilify.
I have health w/severe panic/anxiety attacks after brutal abuse that left a neck full of metal now, & tricompartmental tears in both knees Drs can’t, & won’t replace at this point. I’m an alternative health practitioner, & was a top personal trainer. Not anymore though! I began bioidentical hormones 10 yrs ago, but kept telling my doctor I am hypothyroid, & we knew adrenals were getting bad from ongoing stress, plus chronic severe pain added to the mix. This has gone on for 9 yrs now. I have finally found a specialist, but am paying a high cost to do so. But after researching these hormones for yrs, they have never caused cancer, & can rectify just about everything including getting off 2 deadly meds for pain, & panic. I highly recommend Dr Colberts 2019 book on hormones, his Keto zone diet book, & a book by Dan Hale, “The Truth of Bioidentical hormones “. My first appt is June 29th 2020, and I hope to be able to write great news by August/Sept. God Bless.
Be a member of Thyroid UK – ask for your thyroid panels & then put them on there. The members on there will tell you whether or not you have hypothyroidism. The lab ranges given by uk are too wide & it is about your symptoms being alleviated & not what your ranges say. I would seriously think about going on there & once you know from people’s response then privately see an endocrinologist who will be willing to treat your symptoms- the site has a list & they are all qualified but offer T3 aswell as T4. I wouldn’t recommend antipsychotic because they can give you hypothyroidism & also affect it if you have hypothyroidism. Listen to what your body is telling you & I hope by going on Thyroid UK you will be on the path of getting better.
Tammy I’ve left you a reply – not sure if your UK based ? Def get the 9am cortisol test done I would recommend. Let me know how you get on ok – Davina
Could you please provide references.
Thanks
Since 2012, I have been experiencing constant fatigue, brain fog, and headaches. I’ve had NUMEROUS labs done but no one can seem to figure out. My testosterone levels have been up and down for the past 6 years from 530, 370, 265, 730, 710, less than 12, 527, & 440. My TSH along with FT3 are both HIGH. This has been the puzzling part about it. The doctors can’t seem to figure it out. My Cortisol levels are in the lower end range in the morning but increase as the day goes on instead of decreasing like normal. My TPO has been checked twice, it’s normal. I did test positive for inflammation in my body. When I take thyroid medicine it attacks my TSH but not my FT3. Any suggestions on what it could be or any more testing?
Thomas, have your pituitary and hypothalamus checked. You may need to have a pituitary stimulation test. These 2 glands are the command center for all hormone production. There can be several conditions for a malfunctioning pituitary gland. There may have been event that caused Sheehan Syndrome.
According to Paul Robinson’s books about low thyroid, cortisol has nothing to do with conversion, although it does negatively affect T3 performance.
Can someone recommend a doctor who can help with adrenal rhyroid issues l am miserable
Hi there. Is it possible to have TSH levels that are Hypo and then, all of a sudden, go hyper? I am thinking I have Hashimoto’s. My TSH levels have been elevated for past few years, but doc never put me on meds due to it being “within normal range.” This year, at my physical exam, I told her the long range of symptoms that I have had for past years and that they are worsening. I went to endocrinologist last week and left feeling so hopeful that I would finally know what I am battling. She looked and said definitely hypothyroidism and possible Hashi’s. She had me go and do a slew of blood work. I almost cried when my TSH came back at .082!!! I have never had it that low. I know that is within normal range, but it’s never been that low. Also, during this time (last three weeks), I have had flare up of hyper symptoms (palpitations, rapid heart rate, insomnia, etc.) When I am hypo, my symptoms and flare ups are different (severe brain fog, severe joint pain, extreme fatigue, feeling like can’t swallow, etc.) I was so upset to see this number as I feel that this is putting me back at square 1. I don’t want to be sick, I want to be healthy, but I also know something is very wrong with my body and I need answers so I can start a path to wellness. I go back to endo on 1/29 (she will also do thyroid ultrasound as she felt enlargement on left side), but I was just wondering if this TSH test puts me back at square one or normal with Hashi’s?
I need help with adrenal rhyroid pro lens my end took me off levothyroxine because l was feeling hyper symptoms but blood came back ok l have blood sugar low sometimes high came someone help me l have brainbrai for dizzy shaky tired heart racing l feel l still need to take the LevioLeviothyrocine. I need help
Hi Kimberly,
It happened to me for years as well – alternating between a set of hypothyroid symptoms and hyperthyroid symptoms. This was happeneing while doctors were trying to diagnose me. It was torture. I would spend weeks not sleeping at all or weeks sleeping for 12-14 hours!
This was not just in my head! I also had abnormal hyPOthyroid blood tests and hyPERthyroid blood tests every three months or so like clockwork. I was not taking any thyroid or other medication.
I was eventually put on synthetic thyroid meds and they did nothing for the hypo-hyper-thyroid “storm”. My endo recommended removing my thyroid surgically as she thought that the destroying of my thyroid might take years. I decided not to do it and tried NDT (along with a AIP diet and lifestyle change). This eradicated the issue and pretty much all my symptoms too! I have never had hyperthyroid symptoms or blood tests since on NDT.
Ask for a copy of your blood tests, especially the antibodies. Which ones do you have – if any? Have they increased over time?
Very important, if you smoke (even a little), you need to stop as this will “mask” your true TSH. Other patients had warned me about this and I did not take them seriously at first. My TSH was “normal” (but I had symptoms and elevated antibodies) until I stopped smoking. After four months, my TSH went to 17.1, three months later it was suppressed, etc
Also, taking the pill made the whole hypo-hyperthyroid switch worse for me (if I remember correctly estrogen binds to the same proteins used by the thyroid hormones)
Hope this helps! And good luck!
Just wanted to clarify what I wrote about the birth control pill (also valid for other oral estrogen pills). The estrogen causes an increase in TBG (thyroxine-binding globuline). TBG binds thyroid hormones. So more TBG, less free thyroid hormones for use in the body if this makes sense.
Hmmm…my doctor told me there is no way to measure cortisol levels. I think I’ll talk to my endocrinologist about all this. I know something’s up with me. I have had constant stress for years at a time due to alcoholic husband. He’s out of the house now and I’m trying to get my stress under control. It’s very difficult to stop feeling it since it went on for so long. It feels like my body is addicted to it so that when I get it relaxed, something pops into my head and I’m off to the races. Alanon is helping, but insomnia, depression, and pain are ever present. I medicate for all and would love to get off the prescription merry go round and to the bottom of what’s going on.
Hi Patti, A Yale-trained MD wrote this article about adrenal health for Hypothyroid Mom. I mention this because it may be that your doctor will be more open to reading information from a fellow doctor.
https://hypothyroidmom.com/10-signs-you-have-adrenal-stress-and-natural-treatments-for-it/
I have dealt with a myriad of symptoms since they removed my thyroid in 2012. To say that I was losing my mind with the pain and mental confusion is an understatement. As a result I ended up becoming extremely depressed. After yet another unsatisfying visit with my doctor where he offered me more medication to treat the symptoms, I took to the internet and found several great websites. One thing that was suggested was to take my thyroid at night rather than first thing in the morning. I read that cortisol levels peaked by about 8 a,m, and I had been taking my medication between 6 – 7:30 a,m,, so I changed it up to 1/2 of levothyroxine between 1-2:30 p.m. and the other 1/2 around 7:30 p.m., making sure to take on empty stomach and wait at least 1 hour before eating anything. For me it has been a true transformation. I am feeling like the old me. The pain and confusion and depression began to clear almost immediately. I am 9 weeks now with the new dosage and I sleep through the night, have energy in the morning and generally feel healthy. That is huge if you knew where I was coming from. I wish everyone dealing with thyroid issues the best, but don’t give up trying. Doctor’s don’t always understand the problem of how to deal with them, but there are solutions.
Hi! I am a newbie to stage 3 adrenal fatigue and extremely low progesterone. Ugh! I also have epilepsy, which only complicates the situation. I haven’t had a seizure in 6yrs. They are a few and far between! Knock on wood. Anyway, my doctor has put me on 10mg of hydrocortisone in the morning, when I feel my worst and 5mg mid day. Also progesterone cream. I have extremely low cortisol in the morning. It’s pretty much low most of the time. I feel much better in the evening when my levels are in the normal range, but I can’t sleep at all. I would do anything to not take these steroids, but I know I’m in a late stage adrenal fatigue. Should I ask my physician if I can also supplement while I’m on hydrocortisone to be able to ween off them?
Thank you,
If only our docs were “lucky” enough to have hypothyroidism…the cure would be right around the corner all though then all the doctor’s jobs would be in trouble for giving out the secret to healthy lives with a bad thyroid… Kind of like messing with FDA and big Pharma nobody wants to give up to secret although I’m beginning to believe that using a little herb now and then helps reduce stress and therefore may help the rest of the symptoms..
I am so sick and tired of going in circles. Two Dr’s (1 is an Endocrinologist) all say my numbers are “normal”. I know its “off” I can feel it! I asked my Dr about taking a multi vitamin, pro-biotics and omega 3’s to help get me balanced and she told me NO! I even found vitamins for thyroid health. I also just learned how having hypothyroidism can raise your bad cholesterol and actually lower your good. I am so disgusted with the medical community. I read information from medical journals and show it to my Dr and my plea to change my treatment was still dismissed.
Not surprising…
Please visit Amy Meyers website! Be your own advocate! I was just diagnosed with Hyperthyroidism/Graves disease & she has great information, books & supplemnts.
I agree Misty. Dr. Amy Myers has an incredible website and books. You’ll love this article that I recently published by her at Hypothyroid Mom.
https://hypothyroidmom.com/understanding-the-true-cause-of-autoimmune-disease/
Just a suggestion. Ask them if they will do an acth stimulation test. Cortisol levels may be normal, but your body isn’t processing it right
Ty Bollinger has an extremely good site, and has a video about this. his site is called (a bit off puttingly) The Truth about Cancer.
He has just done a very good investigation into thyroid and its vital relationship to IODINE.
I think it might turn some things around for you
The thyroid is the only gland in the body that needs iodine to function.
Have you tried organic nascent iodine? I strongly reccommend you research this.
I’m hypothyroid and have low cortisol level and low Ferritin level. I was on synthroid and cytomel but my heart felt like it was going to jump out of my chest so I quit taking them. Im taking progesterone and estrogen supplements plus Endocrine supplements and a heart pill due to my thyroid problem. My LDL is too high. I don’t know how to eat properly and I hate this disease. I have lost twenty two pounds since November. What am I going to do?
Interesting. While high or low free cortisol levels seem to have a direct impact on thyroid function, would the opposite be true? Would taking thyroid hormones cause changes in cortisol levels?
For example, if someone has low free cortisol levels in the morning, would giving T3 early in the morning (3:30 – 4:30am) help to raise morning cortisol levels? And if that person also had high free cortisol levels in the afternoon and at bedtime (creating insomnia in a big way), would taking T3 at around 2:00pm somehow bring down the cortisol levels?
I mention T3-only as I’ve seen in lab results where increasing T4 tends to cause an increase in Reverse T3, suggesting the presence of high cortisol levels.
Another thought. While I agree it’s important to utilize the adrenal saliva test, would it also be useful to track fatigue patterns during the entire day as a way to roughly interpret cortisol levels? I’ve noticed that sometimes I feel more energetic in the afternoon; other times it’s the other way around.
I have consistently high levels of cortisol (tested within the last year) due to chronic pain. I’m currently taking Ashwaganda…doesn’t seem to be changing my life. Can you recommend anything else? I’ve taken…DSF, Total Cort, Cortisol Manager and other stuff by neuroscience. I have terrible pain spikes, so I know that’s the stressor….
Hello!
I read your question today and I have the EXACT same problem. It was great to find a sister!! Did you ever resolve your pain and cortisol issues?
I have had some success. If you get this please let’s talk!
Phyllis
[email protected]